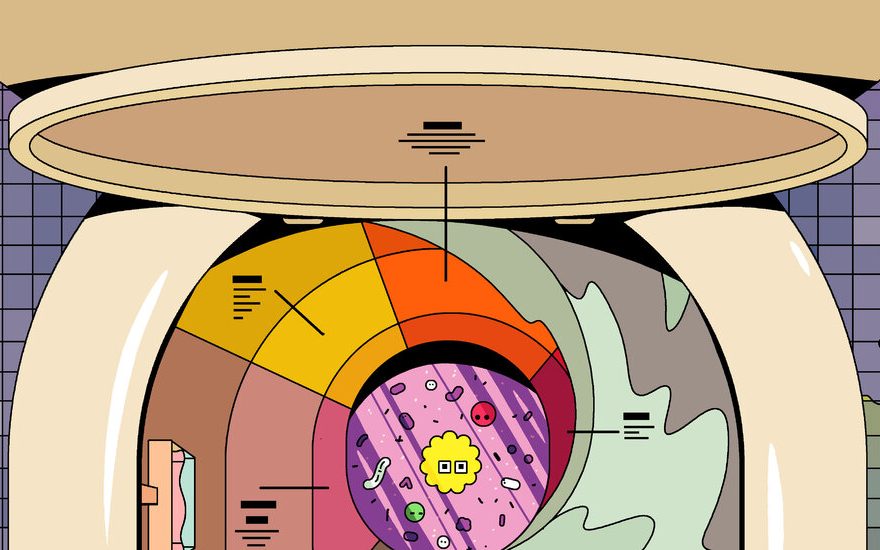
The failure to control the coronavirus pandemic has in many ways been a failure of real-time health data. Worldwide, clinical testing has not identified enough cases, or returned results fast enough, to enable either individuals or health officials to slow the surges without lockdowns. In private, however, nearly everyone does produce a biological sample every day that is then voluntarily sent to a central location to be processed — when they flush the toilet. And fecal waste carries with it a great deal of information about the people who generated it. “If you want to really understand what’s going on in a city on a basic chemical, biological level, you should be looking at the wastewater,” says Eric Alm, a co-director of the Center for Microbiome Informatics and Therapeutics at M.I.T. and the scientific director of Biobot Analytics, a company that collects health data from sewage.
As early as March, evidence began to emerge that the coronavirus is shed in stool and can be detected in sewage. Beginning on March 18, Alm and his colleagues compared a week’s worth of coronavirus concentrations in sewage from an urban treatment facility in Massachusetts with clinical diagnoses in the same area. The wastewater concentrations seemed startlingly high when set beside the number of cases, they reported in the July/August issue of mSystems, a journal from the American Society for Microbiology; to study why, the researchers waited several months and looked at waste samples taken from January to May. The virus first appeared in the sewage on March 3, increased significantly between mid-March and mid-April and then declined.
These changes preceded rises and falls in the number of positive tests by four to 10 days. According to another study by Alm and colleagues (which is a preprint, yet to be peer-reviewed), they have inferred that infected people may shed extremely high amounts of virus in their stool before they show symptoms — if they have them at all — and lower amounts later on. Similar results were reported in a paper published in the October issue of Nature Biotechnology. Jordan Peccia, a professor of environmental engineering at Yale University and his colleagues found that in New Haven an increase in the concentration of virus in sewage preceded by six to eight days an increase in the number of positive test results.
The findings in these papers suggest that sewage surveillance could warn public health officials of an uptick in cases about a week before clinical-testing data alone could, enabling them to issue advisories or implement closures sooner. This would give those measures a better chance of working. Had such monitoring been available early in the pandemic, we might have realized that the virus was spreading within communities on both coasts sooner and been better able to forecast where emergency medical workers and scarce supplies like personal protective gear and ventilators would be needed. “You would want any additional information you could get about the severity and location of the virus,” says Ted Smith, an associate professor of medicine and director of the Center for Healthy Air, Water and Soil at the University of Louisville Christina Lee Brown Envirome Institute. Early diagnostic testing was so limited, Smith says, that “our ability to see the prevalence of the virus was really compromised.”
Though uncommon, monitoring sewage for other infectious diseases has proved useful elsewhere. In 2013-14, Israel experienced a poliovirus outbreak. At first, no one noticed; the country believed it had eradicated the pathogen through vaccination. Polio can cause paralysis, but a vast majority of those who get it, typically through exposure to fecal matter from infected people, experience no symptoms. That means poliovirus, like the coronavirus, can circulate widely before being identified. Israel, however, was monitoring its wastewater for poliovirus. Once alerted, health officials quickly immunized a million children, halting the outbreak before any cases of paralysis were reported.

On a small scale, effluent from individual buildings — college dorms, prisons, nursing homes and homeless shelters — is increasingly being surveilled for coronavirus. “When you have congregate living, there’s no question about its utility,” Smith says. Indeed, more than 140 universities around the world have begun monitoring wastewater, according to a dashboard maintained by the Covid-19 Wastewater-Based Epidemiology Collaborative. In those settings, where the transmission risks are high, it’s crucial to quickly identify and isolate positive cases. Testing a daily sewage sample from a building, Smith adds, is a “completely passive and much more cost-effective” way to make sure the inhabitants are virus-free than giving them diagnostic tests every few days. If the virus is detected in sewage, then follow-up diagnostic tests can be administered. In August, the University of Arizona made news when, using this process, it identified and successfully quarantined two asymptomatic students during the first week of classes.
On a larger scale, tracking sewage can serve as a check on whether testing regimens are correctly capturing the spread of the virus in given locations. “Many people will say, ‘There’s not an outbreak, we’ve just increased testing,’” Peccia says. “The wastewater doesn’t know where testing has increased.” In other words, sewage findings that mirror patterns seen in clinical-test reports reinforce their accuracy. Furthermore, while testing sites are often centralized, drawing users from a wide geographic area, sewage can be traced to specific neighborhoods, potentially providing more detailed information about the distribution of the virus. In their preprint, Alm and colleagues noted that in ZIP codes around Boston, the amount of virus present in sewage was not correlated with the number of people who lived there, as they had expected. Rather, the wealthier a neighborhood, the less virus in its effluent. That kind of information could allow local officials to more efficiently direct limited resources to disproportionately affected areas, whose residents may also have less access to Covid testing.
Surveillance could also “exacerbate and compound existing social inequalities,” Alm and co-authors note in a separate July paper in Water Research. Residents from heavily impacted regions could conceivably face harsher restrictions and penalties than, or discrimination from, those who have less exposure to the virus.
The larger the watershed being sampled, the more “anonymous” each fecal contribution becomes. That can alleviate privacy concerns but also make it harder to interpret and act on the results. In the case of coronavirus, for example, it’s still unclear how to estimate the number of individual infections that contribute to a given viral concentration in sewage. For starters, the amount of virus an infected person sheds in stool “can vary by six orders of magnitude,” says Kyle Bibby, an associate professor of civil and environmental engineering and earth sciences at the University of Notre Dame. “If my partner and I are sick, I might be extruding a million more times the virus than they do.”
It is also unknown how comparable sewage data from different regions are. Flow rate, collection methods and other variables can influence results. (The tests detect viral RNA, not an intact germ. “It’s really important people understand,” Bibby says, that it “doesn’t mean the water is infectious.”) In August, the C.D.C. announced the creation of a National Wastewater Surveillance System (N.W.S.S.) to collate local findings. “This is the first time that there has been a large coordinated use of wastewater surveillance in the United States,” says Amy Kirby, the head of the unit.
This sort of system could be valuable in ways that go far beyond catching outbreaks of infectious disease. Sewage monitoring could look for signs of antibiotic resistance, diabetes prevalence and other conditions that are hard to capture outside a hospital setting. Before the pandemic, Smith was checking sewage for signs of air pollution that can be found in urine, and Alm was detecting opioid use. The N.W.S.S. lead scientist, Mia Mattioli, says, “We really envision this being a long-term data-surveillance source” that will outlast the current pandemic.
Source: Read Full Article